The Hidden Danger Lurking in Your Hospital: Why Ignoring Staff Burnout Could Be Fatal

INTRODUCTION: A Crisis in the Shadows
Amid the hustle of a busy hospital rests a burgeoning crisis—staff burnout. As patients continue to receive care and recover, healthcare workers are experiencing increased stress, emotional fatigue, and mental exhaustion. The potential spillover of this hazard not only endangers healthcare professionals but also jeopardizes patient safety and significantly threatens hospital effectiveness. Burnout is not just an individual problem; it has systemic implications that hospitals can no longer afford to overlook.
This article highlights the impact of burnout, including its cascading consequences for hospitals and patients, and the concrete steps that can be taken to counter it.
Exploring Burnout: A Deeper Dive
Burnout is more than exhaustion. The World Health Organization (WHO) describes it as a syndrome that arises from chronic workplace stress that has not been successfully managed. Burnout for healthcare staff manifests in three major areas:
1. Emotional Exhaustion
Feeling mentally fatigued from caring for patients.
Struggling to summon energy to tackle daily challenges.
2. Depersonalization
Increasing disconnection from patients, colleagues, and duties.
Developing tendencies toward cynicism or negativity.
3. Lower Sense of Achievement
Feelings of ineffectiveness and loss of confidence.
These symptoms lead to more mistakes, poor work output, withdrawal from the profession, and toxic workplace environments.
The Cost of Burnout: Beyond the Individual
1. Impact on Patient Safety
Burnout leads to increased medical errors, delayed treatment, and suboptimal care. For instance:
– A tired nurse may miscalculate a medication dosage.
– An overworked doctor may overlook critical diagnostic information.
These errors have tangible impacts on patient health and safety.
2. Workforce Management: High Employee Turnover and Recruitment Issues
Burnout is a leading cause of high turnover rates in healthcare. When experienced professionals leave, hospitals face:
– Rising expenses for recruiting and training new employees.
– Loss of institutional knowledge and expertise.
– Lower morale among remaining employees.
3. Financial Strain on Hospitals
Burnout is expensive. Studies estimate replacing one nurse costs between 1.5 to 2 times their annual salary. Additional financial burdens arise from:
– Fines for poor patient outcomes.
– Inefficiencies caused by frequent staff turnover.
4. The Decline of Workplace Culture
Burnt-out employees contribute to a toxic work environment characterized by:
– Poor communication.
– Lack of collaboration.
– Erosion of trust between employees and management.
The Ripple Effects of Burnout: How It Affects Patients
Patients are the silent victims of staff burnout, experiencing the following consequences:
1. Extended Waiting Times
Burnt-out employees are less efficient in managing workloads, leading to longer waits for treatment.
2. Decreased Empathy
Emotionally exhausted providers struggle to build bonds with patients, making them feel neglected or undervalued.
3. Repetitive Readmissions
Hasty or incomplete care plans result in avoidable complications, increasing hospital readmissions.
Pinpointing the Triggers: What Drives Burnout?
Burnout doesn’t develop overnight; it stems from long-term exposure to stressful situations, often worsened by systemic flaws:
1. Overburdened Workloads
Shortages in healthcare staff force existing employees to take on extra work, resulting in physical and mental fatigue.
2. Lack of Autonomy
Many healthcare professionals feel disempowered, with limited control over schedules, workflows, and decision-making processes.
3. Emotional Toll
Caring for critically ill or terminal patients is emotionally draining, particularly when error-free care is demanded.
4. Insufficient Support
Inadequate mental health resources and poor leadership leave staff feeling isolated and undervalued.
The Path to Prevention: From the Top Down
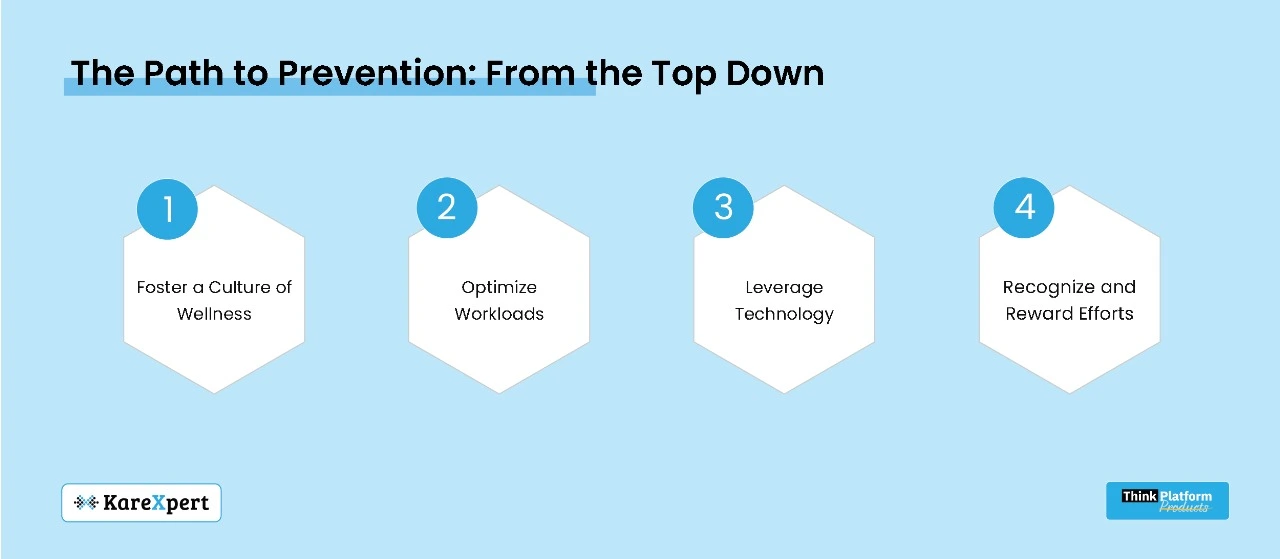
Addressing burnout requires a multifaceted approach involving organizational and individual interventions:
1. Foster a Culture of Wellness
– Management Training: Teach managers to recognize burnout signs and encourage open communication.
– Mental Health Resources: Provide counseling, support groups, and stress management programs.
– Peer Support Programs: Build a sense of community among staff.
2. Optimize Workloads
– Ensure Sufficient Staffing Levels: Recruit resources to distribute workloads effectively.
– Efficient Scheduling: Develop flexible systems to avoid unnecessary overtime and ensure adequate break coverage.
3. Leverage Technology
– Automation: Use digital tools to streamline administrative tasks, allowing staff to focus on patient care.
– Predictive Analytics: Identify high-risk areas and allocate resources accordingly.
– Telehealth Solutions: Reduce the burden on frontline workers by enabling virtual consultations.
4. Recognize and Reward Efforts
Acknowledge contributions with awards, bonuses, or appreciation gestures.
Offer professional development opportunities, including training programs and career progression pathways.
Case Studies: Hospitals Doing It Right
1. The Cleveland Clinic
Implemented a caregiver support program featuring:
– Wellness centers for staff.
– Free mental health services.
– Stress management and resilience workshops.
Results: Burnout levels decreased by 60% in three years.
2. Kaiser Permanente
Adopted AI-driven scheduling tools to optimize shift rotations and reduce overwork.
Results: Improved staff satisfaction and a 15% reduction in nursing turnover.
3. Singapore General Hospital
Introduced mindfulness training for staff, enhancing engagement and patient satisfaction.
Results: 30% reduction in absenteeism due to burnout.
If You Ignore Burnout, You Might Be Sorry
Neglecting burnout is not just irresponsible—it’s dangerous:
– Reputation Damage: Negative patient outcomes and employee complaints tarnish a hospital’s reputation.
– Regulatory Repercussions: Burnout-induced errors can lead to fines and compliance violations.
– Growth Sabotage: A disengaged workforce hampers innovation and adoption of new practices.
Conclusion: A Call to Action
Burnout is a quiet but immense threat that permeates the entire healthcare delivery system. Ignoring it is no longer an option. Hospitals must take bold steps to safeguard their greatest asset—their people.
By promoting a supportive culture, optimizing workflows, and leveraging technology, healthcare organizations can foster staff well-being and high-quality patient care. The price of inaction is simply too great. Reinventing how we think about staff well-being is not just the right thing to do—it is essential for the future of healthcare.
