Revolutionize Your Healthcare Business with NHCX: The UPI Moment for Health Insurance in India

In the landscape of Indian healthcare, digital innovation is setting the stage for transformative changes. One of the most promising developments is the National Health Claims Exchange (NHCX), a pivotal initiative under the Ayushman Bharat Digital Mission (ABDM). This platform is designed to revolutionize health insurance delivery by facilitating a seamless, transparent, and efficient interaction amongst healthcare providers, insurance companies, and policyholders. Here’s a deep dive into how NHCX is turning into the UPI moment for health insurance in India, aiming to significantly enhance the efficiency of health insurance claims and management.
The Genesis of NHCX
With the rapid advancement in healthcare technology and a growing emphasis on digital health records, there was a clear need for an integrated system that could streamline health insurance claims and benefit the entire healthcare ecosystem. Recognizing this, the ABDM, along with the National Health Authority (NHA) and the Insurance Regulatory & Development Authority of India (IRDAI), initiated the NHCX. This platform is intended to act as a digital medium that simplifies the processes of filing claims, settling payments, and accessing medical records.
How NHCX Works: A Digital Bridge for Better Health Insurance
NHCX operates by interlinking three core components of the healthcare and insurance sectors:
1. Healthcare Providers: Hospitals, diagnostic centers, and pharmacies.
2. Insurance Entities: Insurance companies, Third-Party Administrators (TPAs), and state health agencies.
3. Insured Individuals: People holding health insurance policies.
This integration allows for the digital and real-time exchange of information, ensuring that all stakeholders have access to the necessary data to execute and process claims efficiently, make informed decisions, and manage healthcare delivery effectively.
Key Benefits of Implementing NHCX
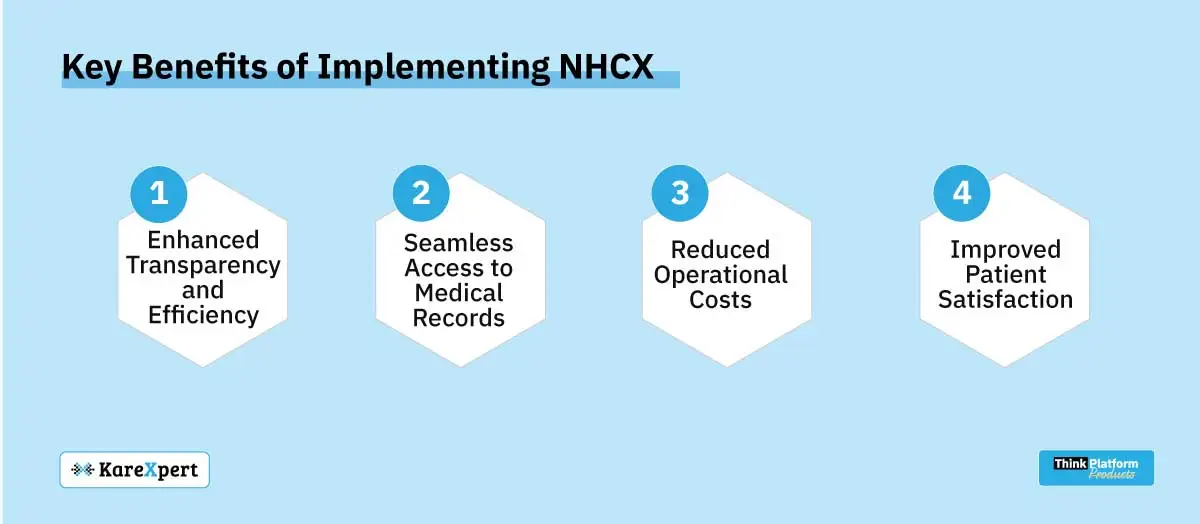
1. Enhanced Transparency and Efficiency:
NHCX ensures that all health insurance claims are processed in a transparent and time-efficient manner. This reduces the likelihood of fraudulent claims and delays in payment, which are common challenges in the traditional claim processing system.
2. Seamless Access to Medical Records:
By digitizing health records and integrating them within the NHCX, healthcare providers and insurers can access up-to-date patient information anytime. This facilitates a better understanding of each patient’s medical history, leading to more accurate claims management and patient care.
3. Reduced Operational Costs:
The automation and digitization of claims processing significantly cut down administrative and operational costs associated with manual paperwork. This not only benefits insurance companies and healthcare providers but also contributes to lower insurance premiums for consumers.
4. Improved Patient Satisfaction:
With faster claims processing and easy access to insurance benefits, patients experience greater satisfaction with their insurance providers. This can lead to higher retention rates and positive reviews for both healthcare providers and insurers.
Challenges and Considerations
While the benefits are compelling, the implementation of NHCX also presents challenges such as ensuring data privacy and security, managing the change from traditional to digital processes, and achieving widespread adoption across all levels of healthcare providers. Addressing these challenges requires robust cybersecurity measures, continuous training, and awareness programs.
The Future of NHCX: What Lies Ahead?
As NHCX continues to evolve, it will likely incorporate more advanced technologies such as blockchain for enhanced security and AI algorithms to predict fraudulent claims and automate claim adjudication processes. The future of NHCX is not just about transforming health insurance claims; it’s about setting a new standard for how healthcare is delivered and managed across India.
Conclusion
NHCX stands as a testament to India’s commitment to improving healthcare through technological advancements. By fostering a collaborative environment among the key players in the healthcare and insurance sectors, NHC Suite is poised to drive significant improvements in health insurance transparency, efficiency, and overall patient care. As this initiative gains momentum, it promises to reshape the landscape of health insurance in India, making it more accessible, understandable, and user-friendly for everyone involved.
Embrace the future of healthcare with NHC Suite and discover how streamlined health insurance management can benefit your facility and patients. Contact us for more information and get ready to transform your healthcare operations with the power of digital innovation.
