DON’T Wait Until It’s Too Late: How Poor Discharge Processes Cost Hospitals and Patients

Section 1: The Cost of Bad Discharges
In many hospitals, we treat discharge as just another administrative task. But this relatively simple step can be the linchpin of patient recovery and hospital efficiency. If not done correctly, the consequences are not only dissatisfaction; it costs hospitals in operational inefficiency, financial penalties, and legal risks. The stakes for patients can be much higher, leading to complications, readmissions, or death. This article explores the hidden costs to hospitals and patients from poor discharge processes and why addressing this issue is imperative, not optional.
The Anatomy of an Ineffective Discharge Process
To appreciate the effect it has, here are the elements that make up a lousy discharge process:
Inadequate Communication
Patients are often told to go home with vague instructions or medical jargon that goes over their heads. This lack of clarity leads to:
– Missed medications or incorrect dosages.
– Ignoring follow-up care instructions.
– Uncertainty around when to seek additional medical care.
Fragmented Care Coordination
When discharge spans multiple departments, such as pharmacy, nursing, and primary care, the gaps in coordination can lead to:
– Delayed legislation or regulation.
– Reports for tests or diagnoses that have not been shared.
– Medications unavailable at discharge.
Not Enough Preparation Done by Patients
Several barriers lead to patients and caregivers leaving the hospital unprepared to manage care after discharge, including:
– Minimal training for wound care, injections, or movement exercises.
– Absence of support resources, like home supplies, or access to helplines.
The Ripple Effect: Implications for Hospitals
1. Increased Readmissions
Hospital readmissions are largely driven by inadequate discharges. Studies have found that patients who do not receive clear discharge instructions are 2.4 times more likely to be readmitted within 30 days.
– Financial Consequences: Readmissions often incur penalties associated with value-based care designs, such as the Hospital Readmissions Reduction Program (HRRP).
– Reputational Harm: Increased readmission rates diminish hospital rankings and patient confidence.
2. Operational Inefficiencies
Delayed or mishandled discharges:
– Site of Care Workups: Higher numbers of beds do not necessarily lead to more admissions; waiting for an available bed is often a primary cause of bed turnover delays.
– Staff Overload: Nurses and administrative staff work additional hours addressing discharge-related errors, contributing to burnout.
3. Financial Losses
The costs of inefficiency and penalties of bad discharges accumulate:
– Loss of Revenue: Disruption of patient flow due to delayed discharges can interrupt revenue cycles.
– Legal Liabilities: Mistakes during discharge can result in malpractice suits, creating additional financial burdens on hospitals.
The Patient Perspective: The Perils of a Bad Discharge
1. Potential Health Risks and Complications
Patients discharged prematurely are at risk of:
– Medication Mistakes: Errors in dosing or failing to take critical medications.
– Infections: Improper care of wounds or failing to notice early signs of infection.
– Delayed Recovery: Missed follow-up appointments extend the healing process.
2. Mental and Psychological Stress
Ambiguous discharge instructions further exacerbate anxiety for patients and their families:
– Caregivers are often left feeling overwhelmed by the absence of useful guidance.
– This can lead to feelings of neglect, which erode trust in the healthcare system.
3. Financial Burden
The cost of readmissions, extra treatments, and missed workdays takes a financial toll that many patients cannot afford.
How to Effectively Run a Discharge Process
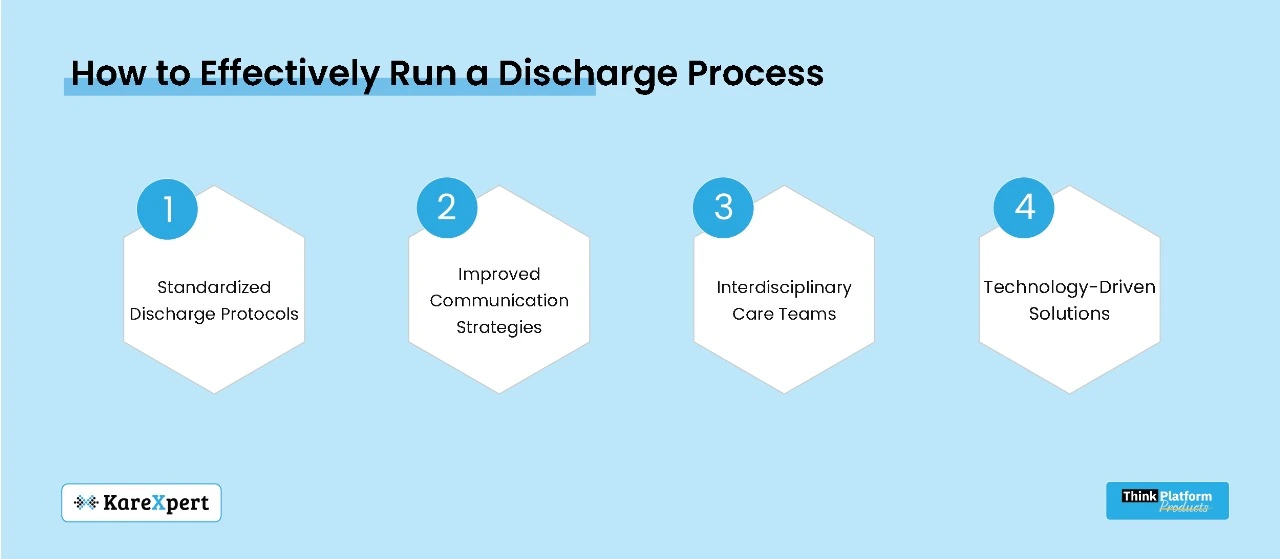
1. Standardized Discharge Protocols
Standardized procedures implemented by hospitals can prevent errors:
– Checklists for Discharge: Ensuring all key processes are performed before the patient leaves.
– Documentation Templates: Discharge summaries often lack important information, but templates can ensure completeness.
2. Improved Communication Strategies
Effective discharges depend on clear communication:
– Teach-Back Method: Patients repeat instructions back, ensuring they understand everything clearly.
– Multilingual Materials: Discharge instructions in multiple languages for multicultural patients.
– Digital Tools: Mobile apps or portals centralize discharge instructions, medication schedules, and follow-up reminders.
3. Interdisciplinary Care Teams
Co-locating doctors, nurses, pharmacists, and case managers promotes holistic management:
– Integrated Pharmacy: Ensures prescriptions are ready before discharge.
– Case Manager Oversight: Manages follow-up appointments and home healthcare needs.
4. Technology-Driven Solutions
Modern tools can streamline and improve the discharge process:
1. Electronic Health Records (EHRs): Automates discharge summaries and links care plans across departments.
2. Telehealth Integration: Enables virtual consultations for post-discharge follow-ups.
3. Predictive Analytics: Targets high-risk patients for readmission to direct additional resources.
Real-Life Examples: Hospitals Hitting the Home Run
.A Multi-Specialty Hospital in Mumbai
Installed a discharge alert system embedded into their EHR, reducing discharge delays by 40%. Results included:
– Reduced Medication Errors: Pharmacist reviews minimized errors.
– Increased Patient Satisfaction: Clear and timely instructions improved satisfaction scores.
Rajasthan: A Rural Health Network
Utilized telehealth for post-discharge care:
– 25% Reduction in Readmissions: Particularly for chronic care patients.
– Elevated Caregiver Involvement: Periodic virtual visits increased caregiver engagement.
The Cost of Inaction
At the hospital level, neglecting discharge optimization leads to:
– Increased Financial Pressure: Fines, inefficiencies, and legal exposure add up.
– Eroding Patient Loyalty: Higher chances of fewer referrals and negative reviews.
– Staff Burnout: Inefficiencies increase stress on healthcare workers.
For patients, the stakes are much higher:
– Avoidable Readmissions: Impacting their health and financial well-being.
– Emotional Toll: Eroding confidence in healthcare providers.
A Road Ahead: Making Discharge Excellence a Priority
Optimizing discharge processes is not just about avoiding penalties—it’s about reimagining care. Hospitals can:
– Invest in Training: Empower staff to handle complex discharge scenarios.
– Adopt Technology: Embrace digital tools to optimize communication and processes.
– Foster Collaboration: Enable interdisciplinary teams to be accountable for the discharge process.
In Conclusion: You Need to ACT NOW, Before It Is Too Late
Weak discharge processes are a time bomb for hospitals and patients. The costs—financial, operational, and human—are too high to ignore. By embracing best practices, leveraging technology, and prioritizing communication, hospitals can turn discharges from a weak link into a point of strength.
Ultimately, improving discharge processes is not merely about operational efficiency but fulfilling the promise of care. No patient—or hospital—should pay the price for preventable failures.
