Streamlining Hospital Discharge: Strategies to Reduce Turnaround Time and Enhance Patient Satisfaction

Efficiently managing patient discharge is a critical component of hospital operations. A streamlined discharge process not only improves patient satisfaction but also enhances operational efficiency and optimizes resource utilization. However, hospitals often face several challenges that can delay discharge, negatively impacting Turnaround Time (TAT) and patient outcomes. This blog delves into common discharge challenges and provides strategic solutions to reduce TAT, streamline discharge processes, and boost patient satisfaction.
Understanding Turnaround Time (TAT)
Turnaround Time (TAT) in the context of healthcare discharge refers to the duration from when a discharge decision is made to the point when the patient vacates the hospital bed. Reducing TAT is crucial for improving hospital throughput and freeing up beds for incoming patients, which in turn optimizes resource use and financial performance.
Common Discharge Challenges
1. Inadequate Communication Among Care Teams
Ineffective communication between doctors, nurses, administrative staff, and other caregivers can lead to misunderstandings and delays in the discharge process. Ensuring that all team members are on the same page is essential for a seamless discharge.
2. Incomplete Patient Education
Patient education regarding discharge plans, medication instructions, follow-up appointments, and self-care procedures can take time. Poorly communicated or rushed education can result in patients returning due to complications or misunderstandings.
3. Delays in Documentation
Completing discharge summaries, prescription orders, and necessary paperwork often encounters bottlenecks, particularly during peak hours. Delayed documentation can significantly extend TAT.
4. Coordination with Post-Acute Care Providers
Arranging follow-up care, home health services, or transfer to rehabilitation facilities requires effective coordination. Delays in securing post-acute care arrangements can hold up the discharge process.
5. Complexity of Arranging Transportation
Some patients, particularly the elderly and those with limited mobility, require special transportation services, synchronizing which can delay discharge.
Strategies to Reduce Turnaround Time (TAT)
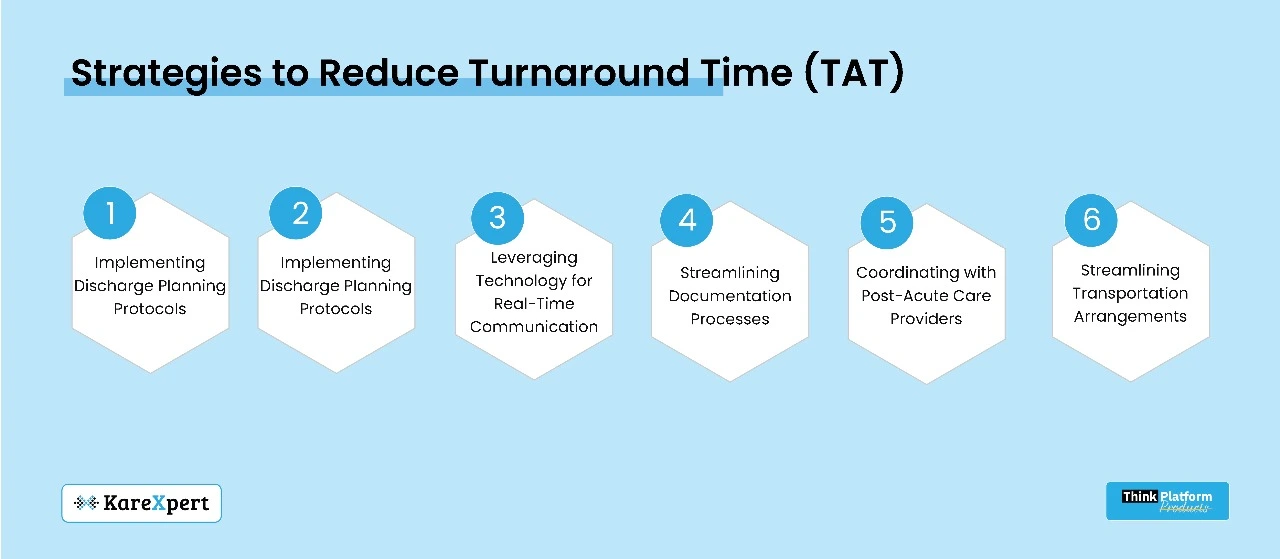
1. Implementing Discharge Planning Protocols
Initiating discharge planning early in the patient’s stay can preempt potential delays. A standardized discharge planning protocol should include clear criteria for assessing discharge readiness and assigning responsibilities across care teams.
2. Leveraging Technology for Real-Time Communication
Adopting centralized communication platforms such as Electronic Health Records (EHRs) or dedicated discharge management software can facilitate real-time updates and coordination among care team members, ensuring everyone is aligned.
3. Streamlining Documentation Processes
Automating documentation with predefined templates, checklists, and digital signatures can reduce paperwork bottlenecks. Real-time documentation by care providers ensures that all necessary paperwork is completed promptly.
4. Enhancing Patient Education and Engagement
Providing comprehensive patient education early in the hospital stay allows for better understanding and preparation. Leveraging digital tools such as patient portals or mobile apps can facilitate continuous education and engagement, improving patient readiness for discharge.
5. Coordinating with Post-Acute Care Providers
Establishing partnerships with post-acute care providers facilitates smoother transitions. Designating a discharge coordinator to liaise with external care providers ensures all arrangements are in place prior to the discharge decision.
6. Streamlining Transportation Arrangements
Collaborating with transportation services in advance and integrating transportation requests into the discharge planning process can minimize delays. Utilizing hospital-owned transport or partnerships with local services can also expedite the process.
Case Study: Success Story
A mid-sized hospital implemented several of these strategies to reduce their TAT significantly. By introducing a centralized discharge planning system, they could streamline documentation and communication processes. They also designated discharge coordinators who worked closely with post-acute care providers and transportation services. As a result, they saw a 30% reduction in average discharge TAT and a significant improvement in patient satisfaction scores.
The Role of Leadership and Continuous Improvement
Effective leadership is crucial in driving change and fostering a culture focused on continuous improvement. Encouraging staff participation in identifying barriers and brainstorming solutions can foster a collaborative atmosphere. Setting measurable goals, regularly reviewing performance metrics, and adapting strategies as necessary ensure sustained improvements in discharge processes and TAT.
Conclusion
Addressing discharge challenges and reducing TAT is essential for optimizing hospital operations and improving patient outcomes. Implementing standardized protocols, leveraging technology, enhancing patient education, and coordinating effectively with post-acute care providers all contribute to a streamlined discharge process. By focusing on these strategic solutions, hospitals can enhance their efficiency, elevate patient satisfaction, and achieve better overall outcomes.
Ready to optimize your hospital’s discharge processes and reduce TAT? Implement these strategies and experience improved efficiency and patient satisfaction.
